By Sarah Wilkinson LLB, BSc (Psychology), Diet and Nutritional Dip.
Your blood – the incredible, life sustaining fluid circulating around your body. The more you know about your blood the better, so lets get educated!
Have you ever been told you need to get a blood test? You are asked to sit down, or, as in my case ly down for fear of fainting, as a needle is inserted into your a blood vessel, and this crazy fluid commonly known as blood is extracted.
Facts:
Blood – slightly viscous, sticky, varies in colour from bright to deep red dependent on oxygen content, has a tightly regulated pH of 7.35 – 7.45, is around 38 degrees celsius, and you have 5-6 litres as male, and 4-5 litres as a female.
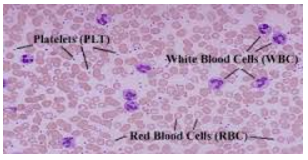
Blood can be divided into three parts:
1 – Red blood cells (RBC) = erythrocytes = O2
RBC account for 45% of your blood. RBC do not have the ability to sustain themselves, therefore last only 100-120 days. RBC main function is to complete gas exchange, delivering oxygen, and removing carbon dioxide from cells. RBC achieve this via haemoglobin (four proteins chains intertwined with an ion molecule).
2 – White blood cells (WBC) = leukocytes, platelets = Immunity
WBC account for 1% of your total blood volume, and are composed of a number of different types of cells responsible for killing bacteria, inflammatory processes, immune responses, antibodies, attacking parasites, viruses, plus so much more! This 1% does some kick arse work in your body! (Check in January 2015 for more info on some of these cells, ways to help yourself, and enhance your immunity).
3 – Plasma
Plasma makes up 55% of your blood, composed of 90% water, plus proteins, electrolytes, lactic acids, gases, hormones, and over 100 other things!
Balancing your blood
Maintaining blood composition is a constant, and critical body function. Blood can:
- become too acidic causing havoc,
- build up in gases and lactic acid,
- RBC count can decrease due to haemorrhage, blood loss, and therefore, tissue perforation decreases,
- can increase in WBC count in response to illness,
- lack clotting factors such as in haemophilia,
- carry excess hormones when they are not being effectively excreted,
- transport excess glucose (sugars),
- inform calcium deposition and bone degradation based on hormonal control of calcium levels, and much much more…
Iron and Anemia
Symptoms of decreased iron include weakness and fatigue, as iron is used by all cells of the body for strength and energy.
Iron is absorbed in the small intestine, and once in the blood stream is bound, transported, used, and stored in bone marrow.
Anemia, the reduction of RBC, deficiency of iron, and therefore, low oxygen in your blood, results in an inability to support normal metabolic processes. Symptoms of Anemia include; fatigue, chills, shortness of breath, and paleness. Those most vulnerable to iron deficiency are pregnant, and lactating women, infants, adolescents, premenopausal women, and vegetarians. (For information of iron rich foods, and how to help facilitate absorption, check in under the nutrition category early next year).
Low on RBC’s – want more? how does the body respond?
The process of blood cell production is hematopoiesis. RBC production is erythopoiesis and is dependent on having adequate B12 vitamins, folic acid, iron, and amino acids. RBC production occurs in your bone marrow in response to a number of factors including hormones, and is tightly regulated given RBC’s have such a limited life span.
Reading you blood levels of iron
So once the blood has been removed, sent to the lab, and then the test returned, make sure you ask for your results to be emailed to you so you can read it with some understanding. Blood tests for iron show result for serum ferritin = the measure of intracellular protein which stores iron, and transferrin = the measure of the iron binding protein found in the blood plasma. Average haemoglobin value per 100ml is 13 – 18 grams in males, and 12 -16 grams in females.
We have only just began uncovering a bit more about your blood. If you think you may be suffering from low iron, or other blood imbalances make sure you see a health practitioner.
References
DermNet NZ. (2014). Iron deficiency. Retrieved December 8, 2014, from http://www.dermnetnz.org/systemic/iron-deficiency.html
Marieb, E. N., & Hoehn, K. (2012). Human anatomy and physiology (9th ed.). Menlo Park, CA: Benjamin Cummings.
Murray, M, T., & Pizzorno, J. (2012). The encyclopedia of natural medicine (3rd ed.). NY, United States of America: ATRIA paperback.
NZ Blood. (2014). Iron and you. Retrieved December 8, 2014, from http://www.nzblood.co.nz/assets/Give-Blood/PDFs/Iron-and-You-111I028.pdf
Stoker, H, S. (2013). General, organic and biological chemistry (6th ed.). Belmont, CA: Broks Cole, Cengage Learning.
Haas, E, M. (2006). Staying healthy with nutrition: the complete guide to diet and nutritional medicine. NewYork, USA: Celestial Arts.
Powers, J, M., & Buchana, G, R. (2014). Iron deficiency anaemia in toddlers to teens: how to manage when prevention fails. Contemporary Paediatrics, 31 (5), 12-17. Retrieved October 12, 2014, from http://web.b.ebscohost.com/ehost/pdfviewer/pdfviewer?sid=6de9ad08-6072-4637-aa12-b287aaae31fe%40sessionmgr112&vid=13&hid=125
Brookdale University Hospital and Medical Center. (2013). Blood bank. Retrieved October 21, 2014, from http://www.brookdalehospital.org/patient-services/blood-bank.html